Pelvic therapy, also known as pelvic floor physical therapy, is a specialized form of physical therapy that focuses on the muscles, ligaments, and connective tissues of the pelvic floor. It is designed to address various conditions and dysfunctions that can occur in this area of the body. During pelvic therapy, a trained therapist will use a combination of manual techniques, exercises, and education to help improve the strength, flexibility, and coordination of the pelvic floor muscles. This can help alleviate pain, improve bladder and bowel control, and enhance sexual function.
Pelvic therapy can help with a wide range of conditions and symptoms related to the pelvic floor. It is commonly used to treat pelvic pain, including conditions such as pelvic floor dysfunction, vulvodynia, and endometriosis. It can also be beneficial for individuals experiencing urinary incontinence, fecal incontinence, and pelvic organ prolapse. Additionally, pelvic therapy can be helpful for women during pregnancy and postpartum to address issues such as diastasis recti and pelvic girdle pain. It can also be beneficial for men who have undergone prostate surgery or are experiencing erectile dysfunction.
While pelvic therapy may involve some discomfort or sensitivity, it should not be painful. The therapist will work closely with the patient to ensure their comfort throughout the session. They will use gentle techniques and gradually increase the intensity as the patient progresses. It is important for patients to communicate any discomfort or pain they may experience during the session so that adjustments can be made.

The duration of a typical pelvic therapy session can vary depending on the individual and their specific needs. On average, a session may last between 45 minutes to an hour. The therapist will assess the patient's condition and develop a treatment plan that includes the recommended frequency and duration of sessions. In some cases, multiple sessions per week may be recommended initially, with the frequency decreasing as the patient progresses.
The number of pelvic therapy sessions needed to see results can vary depending on the individual and the severity of their condition. Some individuals may experience improvement after just a few sessions, while others may require several weeks or months of therapy. The therapist will regularly assess the patient's progress and make adjustments to the treatment plan as needed. It is important for patients to actively participate in their therapy and follow any home exercise programs provided by the therapist to optimize their results.

Pelvic therapy is generally considered safe and does not have any significant side effects. However, as with any form of physical therapy, there may be some temporary soreness or muscle fatigue following a session. It is important for patients to communicate any concerns or adverse reactions to their therapist. In rare cases, individuals with certain medical conditions or complications may need to avoid or modify certain aspects of pelvic therapy. It is important to consult with a healthcare professional to determine if pelvic therapy is appropriate for your specific situation.
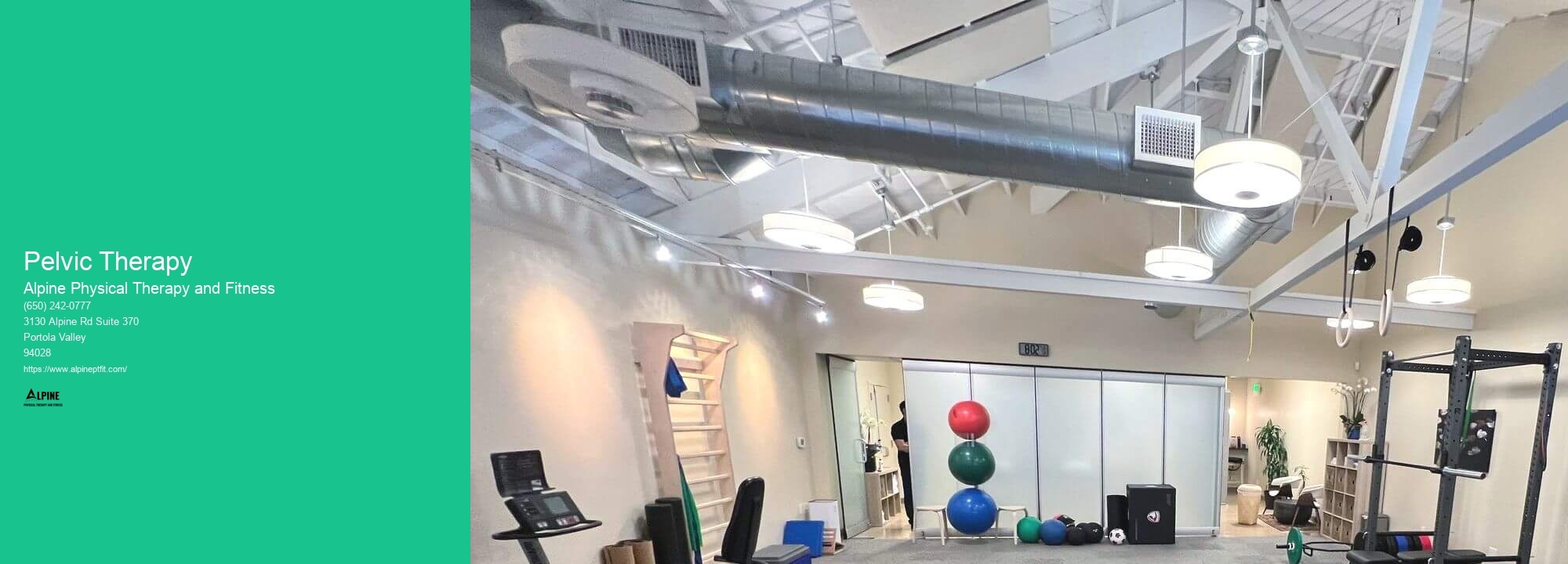
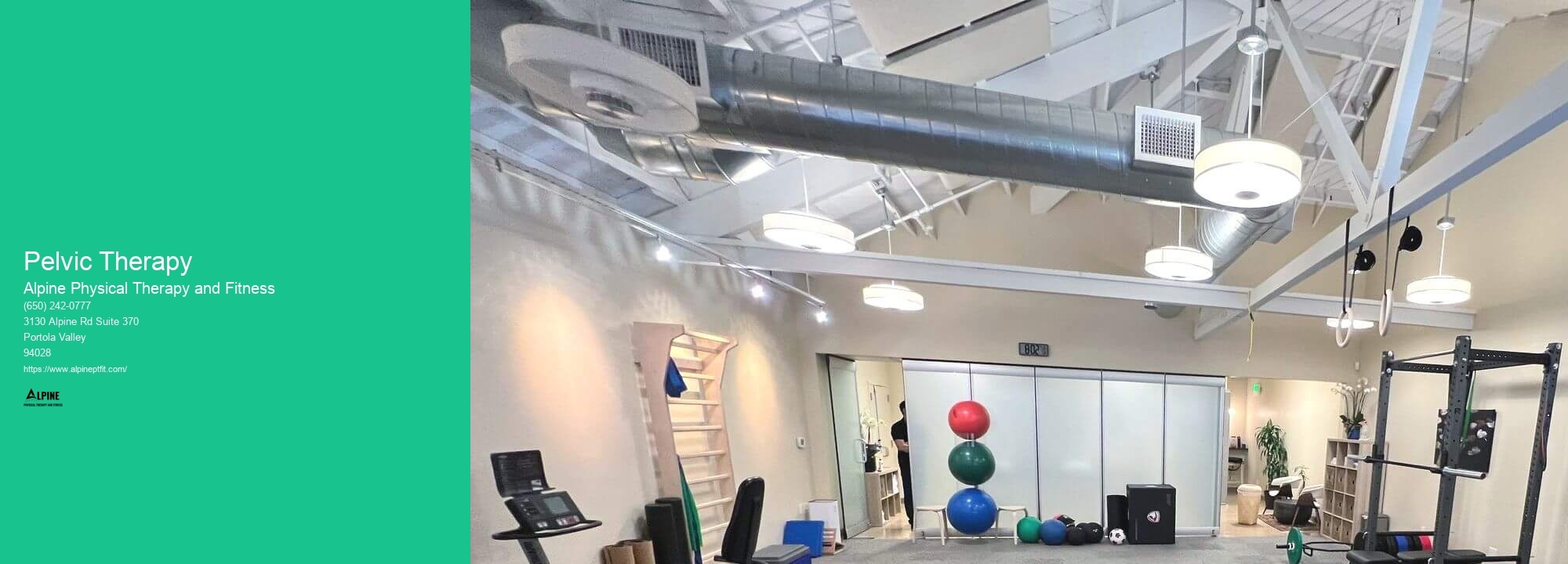
While some pelvic floor exercises and techniques can be done at home, pelvic therapy is typically performed in a clinic under the guidance of a trained therapist. This allows for a more comprehensive assessment and personalized treatment plan. The therapist can provide hands-on techniques, monitor progress, and make adjustments as needed. However, the therapist may also provide patients with exercises and strategies to practice at home between sessions to enhance the effectiveness of the therapy.

Aquatic physical therapy has been found to be highly beneficial for individuals with fibromyalgia. The buoyancy of the water helps to reduce the impact on the joints, allowing for gentle movement and exercise without causing excessive pain. The warm water also helps to relax the muscles and improve circulation, which can alleviate some of the symptoms associated with fibromyalgia, such as muscle stiffness and fatigue. Additionally, the resistance of the water provides a gentle form of resistance training, which can help to improve muscle strength and endurance. Aquatic physical therapy also provides a supportive and safe environment for individuals with fibromyalgia to exercise, as the water provides a cushioning effect and reduces the risk of falls or injuries. Overall, aquatic physical therapy can help individuals with fibromyalgia to improve their physical function, reduce pain, and enhance their overall quality of life.
Yes, the Alexander Technique can be effectively integrated into physical therapy for posture correction. The Alexander Technique is a holistic approach that focuses on improving body alignment, movement coordination, and postural habits. By incorporating the principles of the Alexander Technique into physical therapy sessions, therapists can help patients develop a greater awareness of their posture and movement patterns. This can lead to improved body mechanics, reduced muscle tension, and enhanced overall posture. The Alexander Technique can complement traditional physical therapy techniques by providing patients with tools to consciously adjust and maintain proper alignment and posture throughout their daily activities. By integrating the Alexander Technique into physical therapy, therapists can offer a comprehensive approach to posture correction that addresses both the physical and mental aspects of movement and alignment.
Manual therapy techniques have been shown to be effective in alleviating symptoms of temporomandibular joint dysfunction (TMJ). These techniques, which include mobilization, manipulation, and soft tissue techniques, aim to improve the range of motion, reduce pain, and restore normal function to the jaw joint. By applying specific manual pressure and movements to the affected area, manual therapists can help release tension, reduce muscle spasms, and improve joint alignment. Additionally, manual therapy can help address any underlying musculoskeletal imbalances or dysfunctions that may be contributing to TMJ symptoms. Overall, manual therapy techniques can provide significant relief for individuals suffering from TMJ, improving their quality of life and restoring normal jaw function.
There are several exercises that can help aging individuals maintain their independence. Strength training exercises, such as lifting weights or using resistance bands, can help improve muscle strength and prevent muscle loss. Balance exercises, such as standing on one leg or practicing tai chi, can help improve stability and reduce the risk of falls. Flexibility exercises, such as stretching or yoga, can help improve range of motion and maintain joint health. Endurance exercises, such as walking or swimming, can help improve cardiovascular health and overall stamina. It is important for aging individuals to consult with a healthcare professional before starting any exercise program to ensure it is safe and appropriate for their specific needs.
Yes, there are specialized techniques for treating infant torticollis. One commonly used technique is called passive stretching, where a healthcare provider gently moves the baby's head in different directions to help improve range of motion. Another technique is called active stretching, where the baby is encouraged to move their head on their own through play and exercises. Additionally, positioning techniques such as tummy time and using special pillows or supports can help to alleviate the symptoms of torticollis. It is important for parents to work closely with healthcare professionals to develop a personalized treatment plan for their infant, as each case of torticollis may require different interventions.
Physical therapists play a crucial role in the management of patients with congestive heart failure (CHF). They work closely with these patients to develop individualized exercise programs that focus on improving cardiovascular fitness, strength, and endurance. Physical therapists also educate patients on the importance of regular physical activity and provide guidance on how to safely engage in exercise. Additionally, they may use techniques such as manual therapy and breathing exercises to help improve lung function and reduce shortness of breath. By collaborating with other healthcare professionals, physical therapists ensure that patients with CHF receive comprehensive care that addresses their specific needs and helps improve their overall quality of life.